Colorectal Cancer is the second-leading killer in the U.S., and according to the American Cancer Society (ACS), over 140,000 new cases of colorectal cancer will be diagnosed and over 50,000 will die from the disease in 2018. ACS also notes that “Overall, the lifetime risk of developing colorectal cancer is about 1 in 22 (4.49%) for men and 1 in 24 (4.15%) for women. This risk is slightly lower in women than in men.” African-Americans and Native Americans are at higher risk for developing the disease.
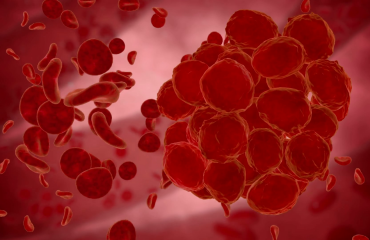
Symptoms of colorectal cancer can range from abdominal pain, rectal bleeding, and chronic constipation to chronic diarrhea and other intestinal problems. An important first symptom is a change in bowel habits. Risk factors include a family history of the disease, a related disease such inflammatory bowel disease or a propensity for developing polyps. Obesity, smoking, poor diet and lack of exercise are also contributing factors.
The ACS has released new guidelines lowering the recommended age for screening from 50 years of age to 45. Yet given the odds of getting colorectal cancer, why then, according to the Center for Disease Control (CDC) are 1 in 3 adults over the age of 50, choosing to skip screening altogether when it could save their lives? The CDC found that up to “23 million people may be at risk for colorectal cancer and not even know it because they’re skipping screening tests.”
One reason may be cost; the others may be the preparation, discomfort and invasive nature of a colonoscopy—considered the gold standard for colorectal cancer screening. The colonoscopy involves a flexible tube—an endoscope–fitted with a tiny camera that’s inserted into the rectum and colon allowing the doctor to view the colon to see whether polyps or other abnormalities are present. This test is the most conclusive but there are risks of perforation, pain and bleeding. Pain is controlled with appropriate short acting anesthesia and perforation is a rare complication. Patients on anticoagulants (blood-thinning medication) must stop them before a colonoscopy and those who take aspirin on a regular basis should stop it two weeks before the procedure.
Another screening test available is the virtual colonoscopy. During a virtual colonoscopy, the doctor does a CT scan of your abdomen and pelvis to create 3-D images which can delineate polyps and other abnormalities inside the colon and rectum. There are downsides— one is the level of radiation a patient might be exposed to during the course of the procedure. Another, should polyps be present, is that a colonoscopy will still have to be performed to view them. Lastly, it is a more costly procedure.
There are in-home blood stool tests — the guaiac fecal occult blood test (FOBT) or the fecal immunochemical test (FIT) which will identify blood in the stool. In general, your primary care physician will do this annually. Furthermore, the test is only an indication that there is intestinal bleeding, and a follow-up visit with a gastroenterologist is needed.
So, what is on the horizon that will make colorectal cancer screening more efficient, less invasive, less costly and infinitely more acceptable to patients?
An Israeli company has developed what they think is the answer. It’s an ultra-low dose ingestible X-ray imaging capsule that requires neither colon cleansing nor sedation as it scans the colon making its way through the gastrointestinal tract (over the course of several days), sending data to a dermal patch receiver. This data is then uploaded and reviewed by your doctor. After the capsule has done its job, it is eliminated naturally.
This technology could reduce colon cancer mortality by screening for precancerous polyps and lesions long before they become malignant and can even be used to monitor at risk patients on a more frequent basis. CheckCap, the company that manufactures this new diagnostic tool has been given CE Mark approval in Europe and is currently working on clinical trials in the U.S. If all goes well, it may reach the market in 2019 or 2020 pending FDA approval.
Several other Israeli companies are also actively developing or marketing colorectal diagnostic tools. For example, Medial EarlySigns, has an artificial intelligence software that can flag data through a series of complex algorithms predicting whether or not a patient will develop colorectal cancer. This allows doctors to assess patient data and intervene sooner if they believe a patient requires treatment or monitoring. The company is currently working with Kaiser Permanente to help diagnose patients within their healthcare system.
Another company is developing a device that clips onto a toilet bowl and according to product information, “the device’s spectral isolation and imaging technologies rapidly analyze solid waste for indicators including blood content, microbiome stability, texture and color that could be warning signs for cancer, irritable bowel syndrome, colitis or Crohn’s disease. It can even distinguish among different people in a household based on Bluetooth signals from their nearby devices.”
Finally, another group of Israeli scientists are adapting tunnel technology used to detect and destroy underground terror tunnels to explore and detect cancer within the tunnels of our colons. No word yet on when this new tool will reach the market.
The options for early detection are varied and growing. So, if you are 45 or older, don’t delay in getting screened.
Strategic Communications Professional/Content Strategist/Marketing Communications Consultant