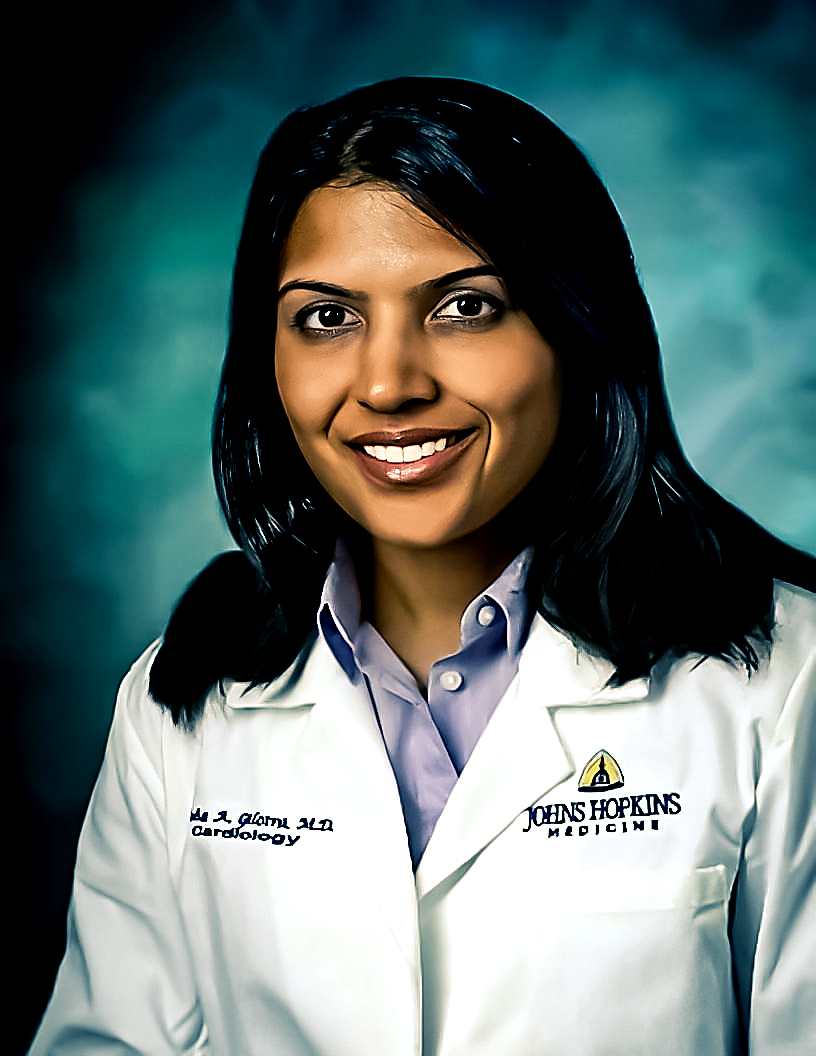
Kamaria C. Cayton Vaught, M.D. is a reproductive endocrinology and infertility specialist in the Baltimore area who specializes in managing disorders related to infertility and the endocrinopathy of female reproductive stages. She has undergone training in the management and evaluation of reproductive disorders such as male and female infertility, PCOS, endometriosis, premature ovarian insufficiency, recurrent pregnancy loss, and advanced surgical techniques in hysteroscopy and laparoscopy. In addition, her unique training also includes genetic counseling, genetic data analysis and interpretation, and preimplantation genetic testing.
Dr. Cayton Vaught completed her combined undergraduate and medical doctor degree at the University of Missouri-Kansas City School of Medicine. She then completed her residency at the University of Maryland School of Medicine, followed by postdoctoral fellowships in reproductive sciences and reproductive endocrinology, infertility, medical genetics, and genomics (REI/MGG) at the Johns Hopkins University School of Medicine. Dr. Cayton Vaught is the first fellow to complete the combined REI/MGG program at Johns Hopkins and one of only a handful of fellowship-trained REI geneticists in the United States.